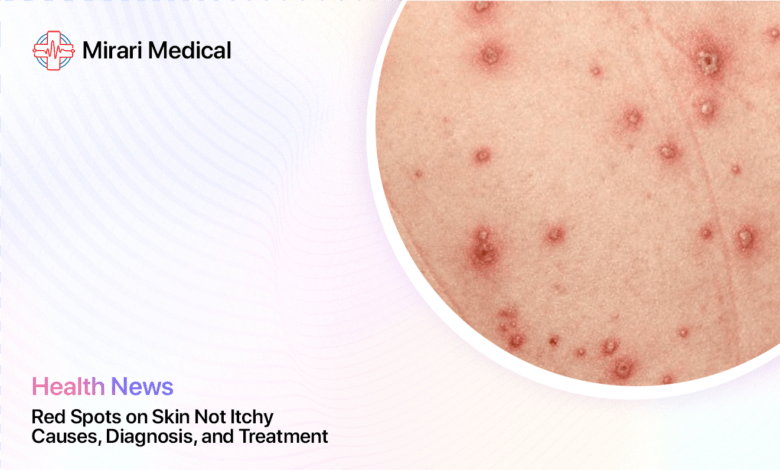
Red Spots on Skin Not Itchy: Causes, Diagnosis, and Treatment
You may be interested
If you’ve noticed red spots on your skin that aren’t accompanied by itching, you may be wondering what could be causing them. While many skin rashes are known for being itchy and irritating, there are actually several conditions that can result in red bumps or spots without the itch factor[1].
As a general rule, any new rash or change in your skin warrants a trip to the dermatologist to get properly diagnosed. However, having some background knowledge on potential causes of non-itchy red spots can help you have a more informed discussion with your doctor. Here’s what you need to know.
Common Causes of Red Spots That Don’t Itch
There are many different skin conditions and factors that can lead to the development of red spots on the skin. Some of the most common causes of non-itchy rashes and red bumps include:
1. Cherry Angiomas
Cherry angiomas are harmless skin growths that occur when blood vessels clump together near the surface of the skin. They appear as small, bright red spots that are typically round or oval-shaped. Cherry angiomas are very common, especially after age 30, and can develop anywhere on the body but are most often seen on the torso, arms, and shoulders[2].
These spots are usually painless and do not itch or bleed. While the exact cause is unknown, they tend to increase in number with age and may run in families. No treatment is necessary for cherry angiomas unless they are cosmetically bothersome or frequently irritated by clothing[3].
Diagnosis and Treatment of Cherry Angiomas
Cherry angiomas are usually diagnosed based on their appearance during a physical exam. Your doctor may use a dermatoscope, a special magnifying tool, to examine the spots more closely. No further testing is typically needed[4].
Treatment is not medically necessary for cherry angiomas but can be done for cosmetic reasons or if the spots are frequently irritated. Treatment options include[5]:
- Electrocauterization: Burning the spot with an electric current
- Cryosurgery: Freezing the spot with liquid nitrogen
- Laser surgery: Destroying the blood vessels with a pulsed dye laser
- Shave excision: Cutting out the spot with a sharp blade
These procedures are usually quick and well-tolerated. Potential side effects include temporary redness, swelling, and scabbing at the treatment site.
2. Keratosis Pilaris
Keratosis pilaris is a very common and harmless skin condition that causes small, hard, red bumps, most often on the upper arms, thighs, cheeks or buttocks. These bumps develop when keratin, a protein in the skin, builds up and blocks the opening of hair follicles. This results in rough, sandpaper-like bumps that may be surrounded by red, inflamed skin[6].
Keratosis pilaris is more common in people who have dry skin or eczema and tends to run in families. It’s often worse in the winter months when skin is drier. While there is no cure, using moisturizers and gentle exfoliation can help improve the appearance of these bumps. Prescription topical retinoids may be recommended in some cases[7].
Diagnosis and Treatment of Keratosis Pilaris
Keratosis pilaris is usually diagnosed based on the appearance and location of the bumps. Your doctor will also ask about your medical and family history, as this condition tends to run in families and occur alongside other skin conditions like eczema[8].
While there is no cure for keratosis pilaris, there are several things you can do to manage symptoms and improve the appearance of your skin[9]:
- Use gentle, fragrance-free cleansers to avoid further irritation
- Apply a rich moisturizer twice a day to help soften bumps
- Gently remove dead skin cells with an exfoliating lotion or wash
- Use a humidifier to add moisture to the air, especially in winter
- Avoid harsh scrubs or picking/squeezing the bumps, which can cause irritation
If over-the-counter remedies aren’t helping, your doctor may prescribe a topical retinoid cream or gel. These vitamin A-derived medications can help unclog pores and reduce the overproduction of keratin. Mild redness and peeling are common side effects but usually improve with continued use.
3. Petechiae
Petechiae are pinpoint red spots that occur as a result of tiny blood vessels called capillaries breaking and leaking blood into the skin. Unlike cherry angiomas, petechiae are flat rather than raised. They often appear in clusters and may look like a rash. Petechiae are usually found on the lower legs, but can develop anywhere on the body[10].
Common causes of petechiae include injuries, straining, certain medications, and low platelet levels. More serious causes like blood stream infections, vasculitis, and leukemia are also possible. If you develop petechiae without an obvious cause, it’s important to see your doctor promptly to determine if an underlying condition needs to be treated[11].
Diagnosis and Treatment of Petechiae
If you develop petechiae, your doctor will start by asking about your medical history and any medications you take. They will perform a physical exam to look for signs of underlying illness and may order tests including[12]:
- Complete blood count (CBC) to check platelet levels and look for signs of infection
- Coagulation tests to check for bleeding disorders
- Blood cultures to check for bacterial infections in the bloodstream
- Urinalysis to check for blood in the urine, which can occur with some bleeding disorders
- Imaging tests like X-rays or CT scans to check for internal bleeding
Treatment of petechiae will depend on the underlying cause. For example[13]:
- If low platelets are the cause, medications to increase platelet production may be prescribed
- Antibiotics will be given if a bacterial infection is found
- Stopping or changing medications that are causing petechiae
- Treating any underlying medical conditions like vasculitis or leukemia
If petechiae are widespread or you also have significant bleeding elsewhere, you may need to be hospitalized for close monitoring and treatment. In severe cases, a platelet transfusion may be necessary.
4. Pityriasis Rosea
Pityriasis rosea is a common, harmless rash that often begins with a single large, slightly raised, scaly red patch called a “herald patch.” Within a week or two, smaller red spots then erupt, usually on the torso and upper arms. They often form a symmetrical “Christmas tree” pattern on the back. The rash may be mildly itchy in some people but is not intensely itchy like eczema or hives[14].
The exact cause of pityriasis rosea is unclear but may be triggered by a viral infection. The rash usually resolves on its own within 6-8 weeks without any treatment. Using moisturizers and taking oral antihistamines or topical steroids can help relieve any itching[15].
Diagnosis and Treatment of Pityriasis Rosea
Pityriasis rosea is usually diagnosed based on the characteristic appearance and location of the rash. Your doctor may order tests to rule out other conditions like syphilis, psoriasis, or eczema that can sometimes mimic pityriasis rosea. These may include[16]:
- Blood tests to check for syphilis and other infections
- Skin biopsy to examine a sample of the rash under a microscope
- KOH test to check for fungal infections
In most cases, pityriasis rosea does not require treatment and will clear up on its own within 6-8 weeks. However, some things can help relieve itching and discomfort in the meantime[17]:
- Taking lukewarm baths with colloidal oatmeal
- Applying unscented moisturizers to damp skin after bathing
- Using over-the-counter hydrocortisone cream to relieve itching
- Taking an oral antihistamine like diphenhydramine (Benadryl) at night if itching is severe
For severe or long-lasting cases, your doctor may prescribe stronger topical steroids or ultraviolet light therapy to help clear the rash more quickly. However, these treatments are rarely necessary.
5. Acne
Acne vulgaris, the most common type of acne, causes red bumps and pustules to develop on the face, chest, and back. Unlike keratosis pilaris, acne spots develop when hair follicles become clogged with oil and dead skin cells, allowing bacteria to grow. Hormonal changes, certain medications, and sometimes diet can contribute to acne breakouts[18].
Acne spots are often tender and painful to the touch but do not usually itch. Over-the-counter acne washes and spot treatments containing salicylic acid or benzoyl peroxide can be helpful for mild acne. More severe acne may require prescription oral or topical medications[19].
Diagnosis and Treatment of Acne
Acne is usually diagnosed based on the appearance of the skin and a history of breakouts. Your doctor will also ask about any medications you take and your skincare routine, as certain products can worsen acne. In some cases, blood tests may be ordered to check for hormonal imbalances that could be contributing to acne[20].
Treatment for acne depends on the severity of the condition. For mild acne, over-the-counter products containing the following ingredients can be helpful[21]:
- Benzoyl peroxide: Kills acne-causing bacteria and helps unclog pores
- Salicylic acid: Helps exfoliate dead skin cells and unclog pores
- Alpha-hydroxy acids: Help exfoliate and improve skin texture
For moderate to severe acne, your doctor may recommend the following prescription treatments[22]:
- Topical retinoids: Vitamin A-derived creams or gels that unclog pores and reduce inflammation
- Topical antibiotics: Kill acne-causing bacteria and reduce inflammation
- Oral antibiotics: Used for short periods to reduce inflammation and bacteria for moderate to severe acne
- Isotretinoin: A powerful oral retinoid reserved for severe, scarring acne that does not respond to other treatments
It’s important to use acne medications as directed and give them time to work. Most treatments take 6-8 weeks to start showing noticeable improvements. In the meantime, be gentle with your skin and avoid picking or squeezing pimples, which can lead to scarring.
When to See a Doctor
While many rashes and red spots are harmless and resolve on their own, there are times when seeing a doctor for an evaluation is important. Make an appointment with your primary care doctor or dermatologist if[23]:
- Your rash is widespread, painful, or blistering
- The rash appeared suddenly and is spreading rapidly
- You have other symptoms like fever, swollen lymph nodes, or joint pain
- Over-the-counter remedies haven’t helped a bothersome rash
- You suspect your rash may be due to a medication or allergic reaction
- Petechiae have developed and you don’t know the cause
- Any rash or skin changes are concerning to you
Rarely, a rash can be a sign of a serious or even life-threatening condition. Go to the emergency room if you have a rash along with any of the following symptoms[24]:
- Difficulty breathing or swallowing
- Swelling of the face or throat
- Dizziness, fainting, or confusion
- High fever or severe pain
- Blisters around the eyes, nose, or mouth
Diagnosis and Treatment
Diagnosing the cause of red spots or a rash involves a thorough assessment by a healthcare provider. Your doctor will ask about your symptoms, when you first noticed the spots, and if you have any other symptoms. They will perform a physical exam to carefully inspect the appearance and location of the spots or rash.
Depending on your symptoms and risk factors, your doctor may also[25]:
- Order blood tests to check for infection, anemia, or autoimmune disease
- Perform a skin biopsy to examine a sample of the rash under a microscope
- Refer you to a dermatologist for further evaluation
Treatment for red spots and rashes will depend on the underlying cause. Some rashes like pityriasis rosea require no treatment and will clear up on their own. Others may benefit from[26]:
- Moisturizing lotions to soothe dry, irritated skin
- Over-the-counter hydrocortisone cream to reduce inflammation
- Oral antihistamines to relieve itching
- Prescription topical or oral medications to treat conditions like eczema or psoriasis
- Antibiotics if an infection is present
- Stopping any medications that may be triggering the rash
If you’re not sure what’s causing your red spots, avoid picking at them or using harsh skincare products that could further irritate your skin. Stick to gentle cleansers and fragrance-free moisturizers until you can see your doctor for a proper diagnosis and treatment plan.
Preventing Red Spots and Rashes
While not all rashes and red spots can be prevented, there are some steps you can take to keep your skin healthy and reduce your risk of irritation[27]:
- Avoid known triggers like harsh soaps, fragrances, and irritating fabrics
- Moisturize your skin regularly, especially after bathing
- Take short, lukewarm showers instead of long, hot baths
- Use sunscreen to protect your skin from sun damage
- Don’t share personal care items like razors or towels with others
- Manage stress, which can trigger flare-ups of conditions like eczema and psoriasis
- See your doctor regularly for skin exams, especially if you have a lot of moles or a family history of skin cancer
When to Worry
Most of the time, red spots on the skin that don’t itch are harmless and nothing to worry about. However, it’s important to see your doctor for an accurate diagnosis, especially if the spots appeared suddenly, are spreading quickly, or are accompanied by other symptoms like fever or pain.
Additionally, any skin changes that last longer than a few weeks or are not responding to over-the-counter treatments should be evaluated by a healthcare professional. Rarely, red spots can be a sign of a more serious condition like vasculitis, lupus, or skin cancer, so it’s always best to err on the side of caution and get checked out.
Your dermatologist can determine the cause of your red spots and recommend the most effective treatment plan to get your skin looking and feeling its best. With proper care and attention, most rashes and spots will clear up quickly, leaving you with healthy, comfortable skin.
The Bottom Line
Red spots on the skin that don’t itch can have many different causes, ranging from harmless skin growths like cherry angiomas to more serious conditions like petechiae or vasculitis. While most non-itchy rashes are nothing to worry about, it’s important to see your doctor for an accurate diagnosis, especially if the spots appeared suddenly, are spreading quickly, or are accompanied by other symptoms like fever or pain.
Additionally, any skin changes that last longer than a few weeks or are not responding to over-the-counter treatments should be evaluated by a healthcare professional. Rarely, red spots can be a sign of a more serious condition like vasculitis, lupus, or skin cancer, so it’s always best to err on the side of caution and get checked out.
Your dermatologist can determine the cause of your red spots and recommend the most effective treatment plan to get your skin looking and feeling its best. With proper care and attention, most rashes and spots will clear up quickly, leaving you with healthy, comfortable skin.
Takeaways
- Red spots on the skin that don’t itch can have many causes, including cherry angiomas, keratosis pilaris, petechiae, pityriasis rosea, and acne
- Most non-itchy red spots are harmless but some can indicate a more serious condition
- See your doctor for any rash that is widespread, painful, spreading rapidly, or accompanied by other symptoms like fever
- Treatment depends on the cause and may include moisturizers, topical steroids, oral medications, or no treatment
- Preventing red spots involves avoiding irritants, moisturizing skin, managing stress, and seeing your doctor for regular skin exams
- If you’re concerned about red spots on your skin, make an appointment with your doctor or dermatologist for an accurate diagnosis and personalized treatment plan
References
- “Slide Show: Common Skin Rashes.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 26 Feb. 2022, www.mayoclinic.org/skin-rash/sls-20077087?s=1.
- “Cherry Angioma.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 8 May 2021, www.mayoclinic.org/diseases-conditions/cherry-angioma/symptoms-causes/syc-20352409.
- Oakley, Amanda, and Jannet Gomez. “Cherry Angiomas.” DermNet NZ, 2010, dermnetnz.org/topics/cherry-angioma.
- Nguyen, Hau V, and Kelly C. Nelson. “Cherry Angioma.” [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532923/
- Bharti, Jitendra, and Surabhi Dayal. “Cherry Angioma.” [Updated 2022 Apr 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544291/
- “Keratosis Pilaris.” American Academy of Dermatology, www.aad.org/public/diseases/a-z/keratosis-pilaris-overview.
- Hwang, Sena, and Robert A Schwartz. “Keratosis pilaris: a common follicular hyperkeratosis.” Cutis vol. 82,3 (2008): 177-80.
- Thomas, Mariya, and Yara A. Khachemoune. “Keratosis Pilaris: A Focused Review.” American Journal of Clinical Dermatology, vol. 21, no. 6, 2020, pp. 869–875., https://doi.org/10.1007/s40257-020-00545-9
- Karadağ, Ayşe Serap, et al. “Treatment of Keratosis Pilaris with Home-Based Glycolic Acid Peels: A Randomized, Double-Blind, Placebo-Controlled Study.” Dermatologic Therapy, vol. 33, no. 6, 2020, p. e14032., https://doi.org/10.1111/dth.14032
- Gauer, Robert, and Elizabeth Wolff. “Petechiae.” [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482331/
- Patel, Anisha A, and Amor Khachemoune. “Petechiae.” [Updated 2021 Sep 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557840/
- Moussa, Mariam, and Rana Mujahed. “Petechiae.” [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537297/
- Stasi, Roberto. “How to approach and treat petechiae.” Hematology. American Society of Hematology. Education Program vol. 2012 (2012): 547-54. doi: 10.1182/asheducation-2012.1.547
- “Pityriasis Rosea.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Oct. 2021, www.mayoclinic.org/diseases-conditions/pityriasis-rosea/symptoms-causes/syc-20376405.
- Mahajan, Khushbu et al. “Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects.” Indian journal of dermatology vol. 61,4 (2016): 375-84. doi:10.4103/0019-5154.185699
- Krakowski, Andrew C et al. “Pityriasis rosea.” [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448120/
- Chuh, A et al. “Prospective case-control study on chills, abnormal urine, myalgia and lymphadenopathy in pityriasis rosea in addition to rash distribution as potential diagnostic criteria.” European journal of dermatology : EJD vol. 15,3 (2005): 195-8. doi: 10.1684/ejd.2005.0471
- “Acne.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 12 Sept. 2020, www.mayoclinic.org/diseases-conditions/acne/symptoms-causes/syc-20368047.
- Zaenglein, Andrea L et al. “Guidelines of care for the management of acne vulgaris.” Journal of the American Academy of Dermatology vol. 74,5 (2016): 945-73.e33. doi:10.1016/j.jaad.2015.12.037
- Elsaie, Mohamed L. “Hormonal treatment of acne vulgaris: an update.” Clinical, cosmetic and investigational dermatology vol. 9 241-248. 24 Jun. 2016, doi:10.2147/CCID.S114830
- Gamble, R et al. “Topical antimicrobial treatment of acne vulgaris: an evidence-based review.” American journal of clinical dermatology vol. 13,3 (2012): 141-52. doi:10.2165/11597720-000000000-00000
- Kaur, Jasmeet, and Kabir Grossman. “Acne Vulgaris and Its Management.” The Journal for Nurse Practitioners, vol. 17, no. 10, 2021, pp. 1233–1239., https://doi.org/10.1016/j.nurpra.2021.08.021
- “Rash 101 in Adults: When to Seek Medical Treatment.” American Academy of Dermatology, www.aad.org/public/everyday-care/itchy-skin/rash/rash-101.
- Reider, Norbert, and Noah Craft. “Rash Evaluation.” [Updated 2021 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549717/
- Gauer, Robert L, and Elizabeth Wolff. “Skin Rashes: A Guide to Common Skin Conditions.” American Family Physician, vol. 104, no. 3, 2021, pp. 249-258.
- “Dermatitis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 13 Mar. 2021, www.mayoclinic.org/diseases-conditions/dermatitis-eczema/diagnosis-treatment/drc-20352386.
- “Skin Care Tips Dermatologists Use.” American Academy of Dermatology, www.aad.org/public/everyday-care/skin-care-basics/care/skin-care-tips-dermatologists-use.
Your trusted source for health info, offering expert advice, news, and tips to stay healthy and informed.





